Dr. Warren’s Blog
Nexplanon
Nexplanon is an implantable type of hormonal birth control that lasts for 3 years. Nexplanon is placed under the skin in your inner, upper arm. This is done in the physician’s office using local anesthesia.
Nexplanon is 99% effective in preventing pregnancy. It works by putting a steady, low dose of hormone (etonogestrel) into the bloodstream, preventing pregnancy for up to 3 years. Hormones in birth control keep an egg from being released by the ovary and prevent sperm from reaching the egg.
The most common side effect of Nexplanon, according to the manufacturers, is a change in your menstrual bleeding pattern. You may experience longer or shorter bleeding during your periods or have no bleeding at all. The time between periods may vary, and in between periods you may also have spotting.
Removal is also done in the physician’s office under local anesthesia by making a small incision in your arm where the Nexplanon is located. This is a straightforward procedure if properly placed. Difficulty can be encountered in removal if the implant is not where it should be.
Side effects include changes in menstrual bleeding patterns, ovarian cysts which usually resolve on their own, headaches, weight gain, breast pain, acne, and flu-like syndrome.
I am pleased to be able to offer Nexplanon as a birth control option for my patients at Marina Shores OBGYN.
Gestational Diabetes Mellitus (GDM)
Gestational diabetes is a carbohydrate intolerance diagnosed during pregnancy.
Approximately 7% of pregnancies are complicated by diabetes, and 90% of these cases are gestational diabetes mellitus (GDM).
Women with GDM have a higher risk of having larger babies. Larger babies often have a more difficult childbirth with problems such as shoulder dystocia and birth trauma. If the estimated fetal weight is greater than 4500 grams, scheduled cesarean delivery is reasonable.
Women with GDM have an increased risk of developing high blood pressure complications during their pregnancy contributing and having babies with low blood sugar and elevated bilirubin levels.
Women diagnosed with GDM can reduce the risk of these complications with a regular exercise program, limiting carbohydrate intake and by taking the appropriate medications. Women with gestational diabetes may also require increased fetal surveillance in the form of ultrasounds, non-stress tests (NSTS), and consultations with an endocrinologist and/or a perinatologist.
Women with GDM should have a follow-up blood test 6-12 weeks after delivery due to their increased risk of having diabetes.
At Marina Shores OBGYN I screen all pregnant patients for gestational diabetes mellitus (GDM). If the diagnosis of GDM is made, appropriate follow-up testing and appointments will be arranged to obtain optimal outcome for you and your baby.
C-section Delivery
Learn more about C- Sections
A C-section refers to the delivery of a baby through an incision in the uterus. C-sections now account for approximately 1 of 3 births.
There are many different indications for a C-section delivery. Most cases of C-sections are done for the safety of the baby and/or the mother. Indications for a C-section that can occur when a woman is attempting a vaginal birth are the baby showing signs of distress, failure to progress in labor, failure of the head to descend in the pelvis in labor, and problems with the placenta or the umbilical cord. Indications for a scheduled C-section can include a breech or transverse (sideways) presentation, medical conditions of the mother, problems with the placenta location, twin pregnancy, a certain infection that can be passed to the baby during the vaginal birth process, prior history of a C-section, and prior history of a fibroid removal.
Most of the time, the mother can be awake during her C-section delivery. And most women do well during their post C-section recovery process. But it is major surgery that has inherent risks of infection, bleeding, injury to the mother and the baby, anesthetic problems, and blood clots in the legs if the mother does not walk regularly during her post-op recovery phase
With the pregnancy following a C-section, there is risk of weakening of the uterine muscle at the uterine scar site. This results in the potential for uterine rupture, so many women schedule a repeat C-section between 39 and 40 weeks with a subsequent pregnancy. There may also be a slightly higher risk of problems with the placenta in subsequent pregnancies.
Women usually leave the hospital on the 4th post-operative day following a C-section. They take oral pain medications starting the day after surgery, and also start walking and eating a regular diet the day after surgery. Women come to the office 2 weeks after their C-section for an incision check, and again 4 weeks after later for their postpartum check. Women need to eat a regular diet, drink plenty of fluids, walk regularly, and not lift anything heavier than their new baby for the first 6 weeks after surgery. Women need to call for heavy bleeding, fever, drainage from the incision and increasing pain.
At Marina Shores OBGYN I am experienced in performing C-section deliveries. I welcome new pregnant patients and will support you and your baby throughout your pregnancy and your delivery process.
Adnexal Mass in Pregnancy
What is an Adnexal Mass?
Adnexal mass in pregnancy refers to a mass or growth in the pelvis, outside of the uterus, which can occur during a pregnancy. Most of these masses are benign (non-cancerous) simple ovarian cysts, less than 5cm in size.
And the majority of these masses found during the first 12 weeks of pregnancy will spontaneously resolve by 20 weeks gestation. But if an adnexal mass persists well into the second trimester and is greater than 10 cm in diameter or complex (being solid or having both solid and cystic areas), removal in the second trimester is recommended. Surgical intervention is to diagnose malignancy or to reduce the risk of torsion (twisting), or rupture.
At Marina Shores OBGYN there is experienced obstetric ultrasound specialist on site for your convenience. She can help to pick up adnexal masses during pregnancy that might otherwise be asymptomatic, thereby allowing for appropriate medical care.Gynecologic oncology consultation is available in the community should there be a concern regarding potential malignancy. Any indicated surgical intervention would be arranged.
Nausea and Vomiting During Pregnancy
Morning Sickness – What is it?
Nausea and vomiting are common problems during pregnancy affecting 70-85% of pregnant women. Also referred to as morning sickness, it commonly begins before 9 weeks of gestation.
Mild cases of nausea and vomiting are treated with lifestyle and dietary changes. Common interventions are eating small meals frequently, avoiding spicy or fatty foods, eliminating iron supplements, and eating crackers in the morning. However, there is little evidence to support these recommendations. Acupressure and ginger may also give some relief, but again, there is little data to support their use.
There is some evidence to support the use of vitamin B6 plus doxylamine. This is a safe first line pharmacologic agent. Promethazine is an additional drug that can be used.
A severe form of morning sickness affecting approximately 0.5-2% of pregnancies is hyperemesis gravidarum. Woman with this condition often cannot tolerate liquids without vomiting and have severe nausea and dizziness. Hyperemesis gravidarum is the most common cause for admission to the hospital during the beginning of the pregnancy.
At Marina Shores OBGYN I offer complete prenatal services and will work with you if you are having problems with nausea and vomiting during pregnancy.
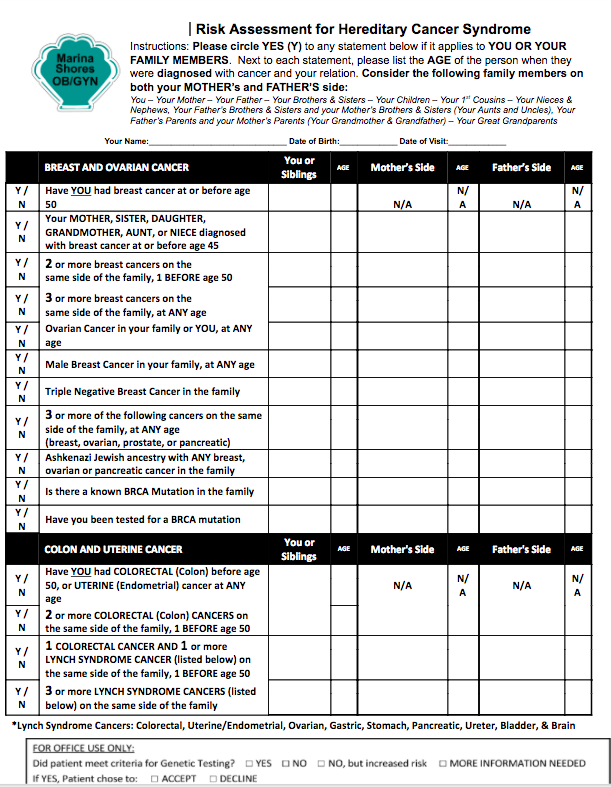
Genetic Testing for Hereditary Cancer
How do genetics affect my risk of developing a certain type of cancer?
Approximately 5-10% of all cancers develop because a person inherits a genetic mutation in a way that encourages the disease to grow. Individuals with these genetic mutations are far more likely to develop certain cancers, often at a much earlier age than the general population.
Medical management of people with a higher cancer risk/hereditary risk can be very different then that for people with a lower cancer risk/general population risk. By working with your healthcare provider, you can determine if your family history suggests increased risk for a hereditary cancer family syndrome. An individual with a personal and/or family history of multiple cancers on the same side of the family, breast, colorectal, or endometrial cancer at age 50 or younger, or rare cancers at any age such as ovarian, male breast cancer, and triple negative breast cancer are examples of red flags to indicate the need to assess for hereditary cancer.
IntroducingmyRisk Hereditary Cancer Test
Here at Marina Shores OBGYN I offer theMyriad myRisk Hereditary Cancer test. This test analyzes 25 genes associated with cancer risks, thereby providing critical information to make optimal medical decisions and take action in building a personalized cancer risk-reduction plan. Myriad myRisk reports can be positive or negative for genetic mutations known to increase cancer risk. Management recommendations for specific cancer risks are generated on the basis of well-established and respected medical guidelines. Ultimately, the information provided allows proper management of your cancer risks.
Heavy Menstrual Bleeding
Why does heavy menstrual bleeding occur?
Many women seek medical care for heavy menstrual bleeding because it impacts their daily activities and quality of life.
The normal menstrual cycle lasts between 21-35 days, and the duration of normal menstrual flow is about 5 days. Excessive blood loss is based upon patient perception.
Diagnosis of Heavy Menstrual Bleeding
The differential diagnosis of heavy menstrual bleeding should be considered when evaluating reproductive age women. Abnormalities to be addressed are evaluation for polyp, adenomyosis, fibroids, malignancy, hyperplasia, blood clotting abnormalities, ovulatory dysfunction, and evaluation of the endometrium.
Evaluation may include blood work, pelvic ultrasound, and biopsy of the uterine cavity. Treatment options are tailored to the individual woman, and may include medical therapy, hysteroscopy with resection of endometrial polyp, hysteroscopy with resection of submucosal fibroid, endometrial ablation, and placement of the intrauterine levonorgestrel-releasing system, a type of IUD, and in some instances hysterectomy.
The patient should be counseled regarding future childbearing and the need for appropriate post-procedure contraception if undergoing surgical procedures for control of heavy menstrual bleeding.
I am able to provide ultrasound and full medical evaluation on site at Marina Shores OBGYN.
Know Your Individual Breast Cancer Risk
Introducing BrevagenPlus Test
At Marina Shores OB/GYN, I am pleased to be offer theBrevagenPlus test. This is a personalized breast cancer risk assessment test that predicts the risk of sporadic, estrogen receptor positive breast cancer. Clinical risk factors and genetic markers are combined to form an integrated risk.
Breast cancer is the second most common cancer among women in the United States. In fact, 1 in 8 women (12%) in the US will be diagnosed with breast cancer during her lifetime.
What are the risk factors for breast cancer?
There are certain risk factors that can increase your risk of developing breast cancer. These risk factors may include things you can change, such as diet and exercise, and things you cannot change, such as your gender and age.
Key risk factors for the most common type of breast cancer (sporadic or non hereditary breast cancer) include: a woman’s age, age at first period, age at first childbirth, history of breast biopsies, and family history of breast cancer.
When detected early, breast cancer has a high survival rate. That is why it is important to know your risk so that steps to reduce your risk or detect breast cancer early can be implemented.
What can I do to reduce the risk of developing breast cancer?
While many breast cancers cannot be prevented, there are things women can do that can reduce the risk of developing breast cancer, or increase the likelihood of early detection. By determining your risk using a Brevagenplus test, we can determine the breast cancer risk reduction and screening plan that is right for you.
How can BrevagenPlus help?
Brevagenplusis a cheek swab-based test that is collected in the office. No blood test is required.
You can make an appointment at Marina Shores OBGYN to have yourBrevagenplustesting done and then to develop a personalized breast cancer risk reduction and screening plan.
Perimenopausal Abnormal Bleeding
What is perimenopausal abnormal bleeding?
As women approach menopause, the incidence of anovulatory uterine bleeding increases. Most bleeding changes at this time are related to normal menopausal transition, but endometrial hyperplasia and cancer need to be ruled out. Perimenopause starts with the onset of cycle irregularity and ends one year after the last menses.
The average age of menopause in developed countries is 51.4, and the average duration of the menopausal transition is 4 years. Pregnancies, although rare, may still occur until one full year without menses. Therefore, for women without contraindications, hormonal contraception, rather than hormone therapy, should be used for pregnancy prevention, menstrual
Treatment for Perimenopausal Abnormal Bleeding
The treatment approach to perimenopausal abnormal uterine bleeding is usually medical, because it is an underlying hormonal abnormality. Surgical therapy is indicated if medical therapy fails, is contraindicated, is not tolerated by the patient, or the patient has intracavitary lesions such as polyps or fibroids.
At Marina Shores OBGYN, I can help to evaluate and manage your issues with perimenopausal bleeding.
Post-Menopausal Bleeding
What is post-menopausal bleeding?
Post-menopausal bleeding refers to vaginal bleeding which occurs after menopause, or one year after cessation of menses. It creates concern for many women.
Most women with post-menopausal bleeding experience the symptom due to atrophic changes of the vagina or of the lining of the uterus, meaning that the tissues have become very thin causing them to bleed easily.
However, vaginal bleeding will be the presenting sign in most women with endometrial cancer, which is cancer of the lining of the uterus. Up to 14% of women with post-menopausal bleeding will have endometrial cancer.
What can I expect at Marina Shores OB/GYN?
Transvaginal ultrasound is a noninvasive diagnostic tool used to measure the thickness of the endometrium/lining of the uterus. Pelvic ultrasound alone may be an adequate initial evaluation. Depending upon the endometrial thickness, biopsy of the lining of the uterus may or may not be indicated.
All reports of postmenopausal bleeding require evaluation. At Marina Shores OBGYN I offer evaluation of postmenopausal bleeding including onsite ultrasound services for your convenience.
Intermenstrual Behavior (IMB)/ Bleeding Between Menses
What causes Intermenstrual Bleeding (IMB)?
IMB refers to bleeding that occurs between menstrual periods. There are multiple potential causes. These causes include growths of the cervix and uterus, abnormal pregnancies, hormonal imbalance, vaginal dryness, pelvic infection, medication and IUD side effects, and pelvic cancers.
There are 1-2% of women that simply have spotting around the time of ovulation, and there is no underlying issue. However, evaluation of intermenstrual bleeding is definitely indicated to make sure that an underlying problem is not overlooked.
What can I expect at Marina Shores OBGYN?
At the time of your office visit, a history will be taken and an exam will be done. Pregnancy testing, hormonal evaluation, testing for infection with cultures, complete blood cell count, pelvic ultrasound, Pap smear/HPV testing, and possible biopsy may be indicated. All of this testing is available on site at Marina Shores OBGYN for your convenience.
Virginia Beach, Meet Dr. Lani Warren
A Quick Introduction
Dr. Lani Warren isa board certified obstetrics and gynecology physician who is passionate about women’s health.Patients visiting Dr. Warren can receive a full range of obstetric and gynecological services. She provides Pap smear procedures, annual gynecological examinations, hysteroscopy and laparoscopy procedures, deliveries, and sterilization.
Risk Assessment for Hereditary Cancer Syndrome
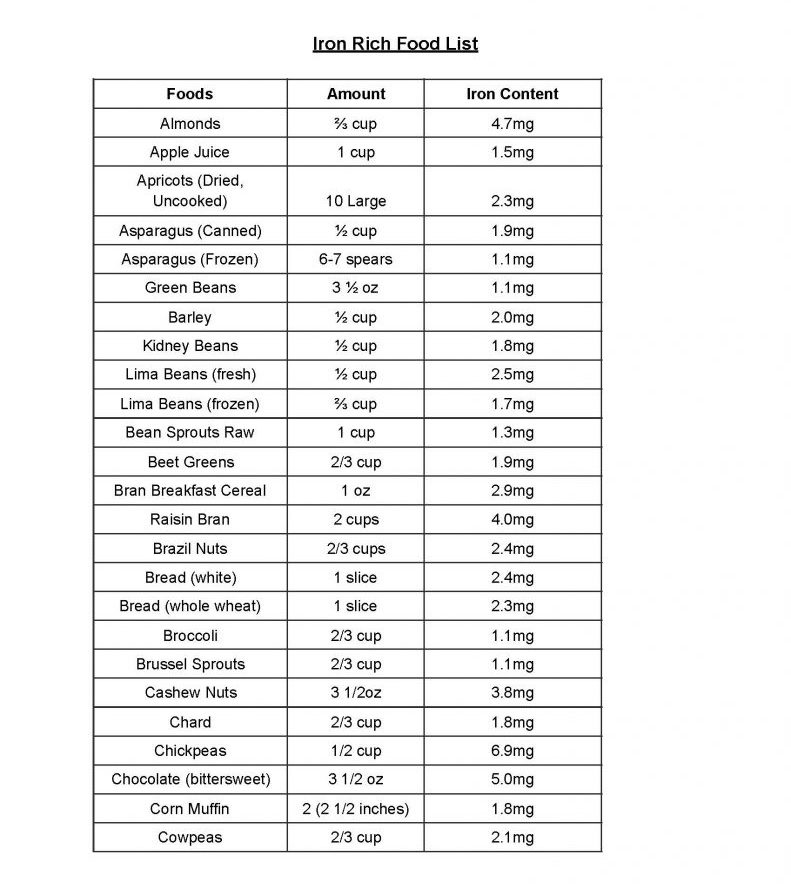
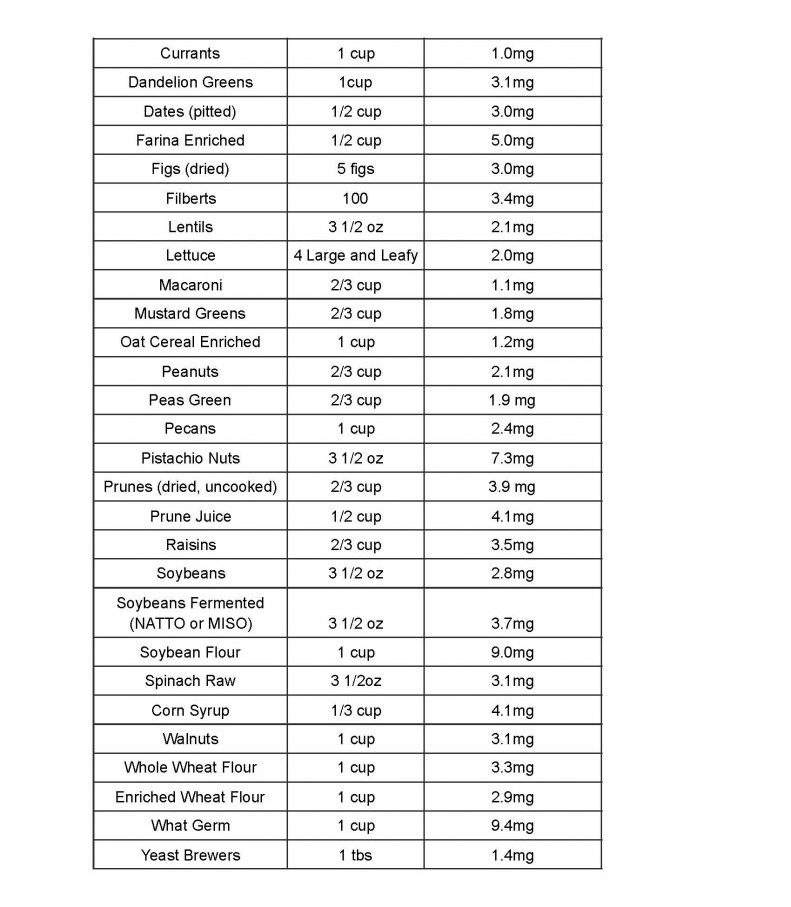
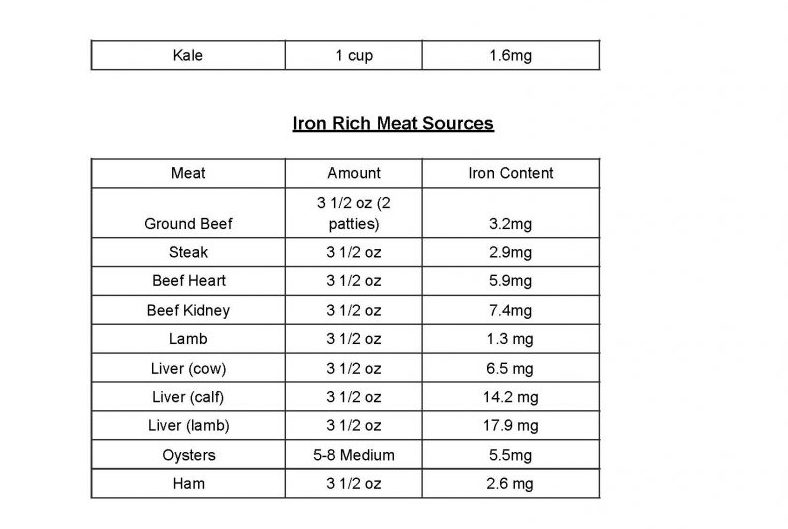
Iron Rich Food List
Approved Over the Counter Medications for Common Pregnancy Issues
PAIN: TYLENOL
ITCHING: BENADRYL, TOPICAL CALADRYL LOTION, AVEENO PRODUCTS
NAUSEA VOMITING: TUMS (REGULAR OR SUGAR FREE), ZANTAC, MYLANTA (LIQUID TABLETS),
MAALOX (REGULAR OR PLUS)
ALLERGIES: BENADRYL, ZYRTEC, CLARITIN (PLAIN CLARITIN)
FLATULENCE: MYLICON
VAGINAL YEAST: MONISTAT, GYNE-LOTRIMIN
COMMON COLDS: ROBITUSSIN (REGULAR, SUGAR FREE OR DM)
CONSTIPATION: INCREASE ORAL FLUID INTAKE, INCREASE FIBER INTAKE (BRAN, GREEN VEGETABLES,
APPLES), COLACE, DULCOLAX, METAMUCIL (REGULAR OR SUGAR FREE), MILK OF MAGNESIA, PERI
COLACE
DIARRHEA: KAOPECTATE, IMODIUM
HEMORRHOIDS: ANUSOL HC, PREPARATION H (CREAM/SUPPOSITORIES)
TOPICAL YEAST (SKIN): MONISTAT CREAM, MYCOSTATIN POWDER, NYSTATIN POWDER
Prenatal Testing Overview
Initial Visit: Prenatal Panel
PAP/HPV, GC, Chlamydia
Urine Culture and Toxicology Screen
Inheritest
12 Weeks: NIPT
16-18 Weeks: QUAD Screen
19-20 Weeks: Ultrasound
28 Weeks: 1 hour
Glucola, CBC
Rhogam if RH Negative
Cord Blood collection information
36 Weeks: Group B Strep Culture
YOU WILL BE SEEN EVERY FOUR WEEKS UNTIL GESTATION, THEN EVERY 2 WEEKS UNTIL 26 WEEKS GESTATION AND THEN WEEKLY UNTIL YOU DELIVER
MORE VISITS AND TESTING SUCH AS BLOOD WORK, ULTRASOUNDS, AND NONSTRESS TEST (NST) WILL BE DONE IF INDICATED
DELIVERY WILL BE DONE AT CHESAPEAKE REGIONAL MEDICAL CENTER. INDICATED PERINATOLOGY CONSULTATIONS WILL BE AT EVMS